Introduction / overview
COVID-19 is highly infectious. Infection control and prevention are critical to protect patients and staff. Administrative controls, environmental controls and personal protection are all key elements of a safe environment. All of these controls rely on vigilance for suspected cases and safe screening, testing and isolating confirmed cases.
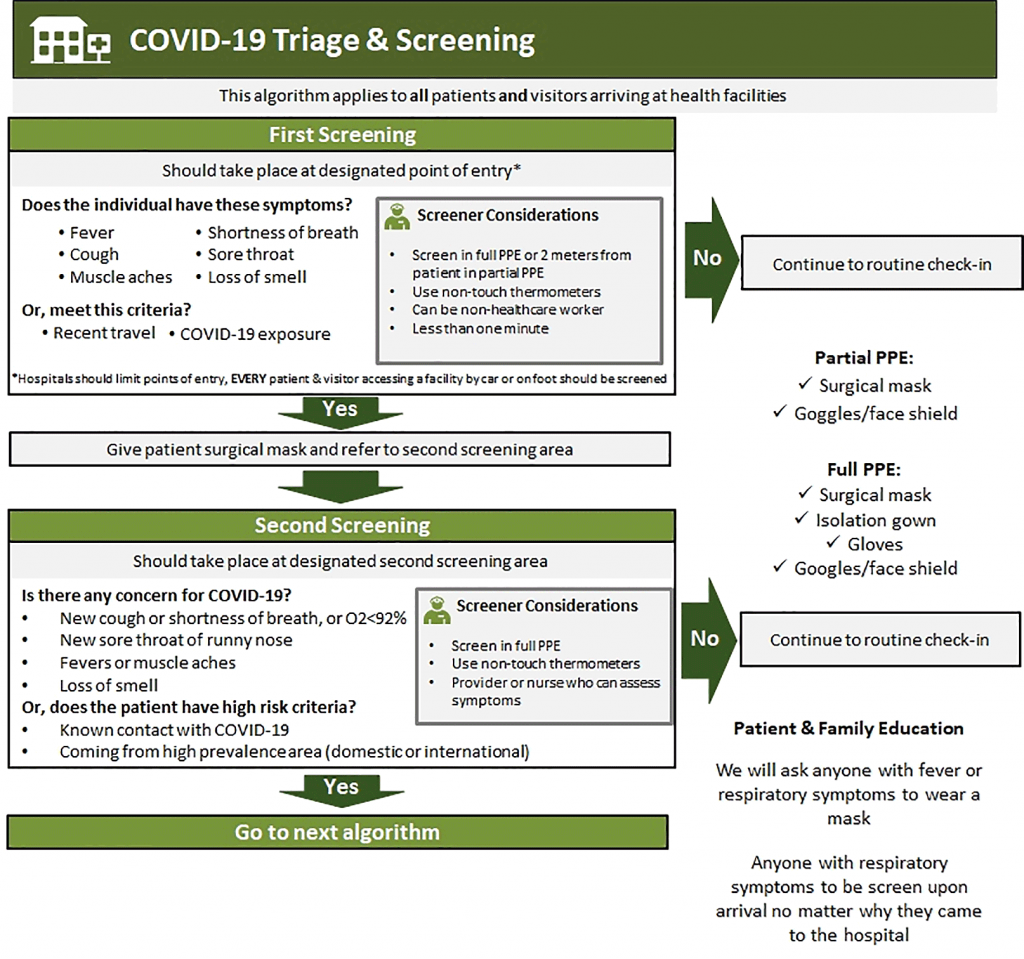
Initial screening
- Separate screening area outside of healthcare facility or at hospital entrance
- All patients entering healthcare facility are screened for fever, cough, SOB, known contact of COVID-19 patient, or recent travel that may place them at risk
- Screener should wear full PPE
- If initial screen positive:
- Immediately place face mask on patient and provide patient with alcohol based hand sanitiser
- Direct patient to triage & testing area
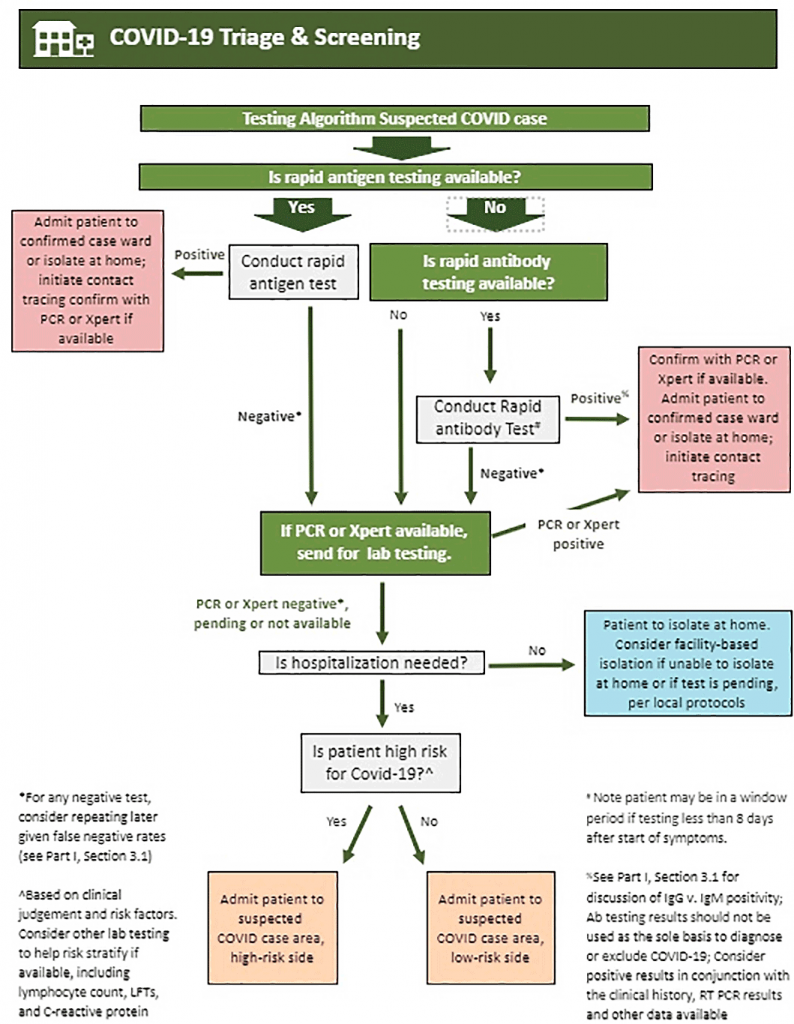
Triage & testing
- Secondary screening space should be separated from other patients
- Providers should don full PPE and observe contact and droplet precautions
- Follow protocols for specimen collection for laboratory testing
- Asymptomatic patients may be directed home with follow up and to self-isolate pending test results
- Symptomatic patients may be admitted to isolation area per protocol
Suspected / probable cases of COVID-19
There should be separate isolation areas for suspected or probable cases who have not yet been confirmed to have COVID-19.
- When a patient comes to a facility with symptoms consistent with COVID-19, known contact with COVID-19, or a history of travel, it is important that IPAC is adhered to. There are two levels of isolation:
- Asymptomatic suspected/probable cases: Known contact or travel history, but no symptoms. Once tested asymptomatic suspected cases may return home with close follow up and instructions to self-isolate pending test results
- Symptomatic suspected/probable cases: Should be evaluated clinically for admission and separated from asymptomatic patients pending the test result
- Presumptive case areas for suspected or probable cases should be separated into low and high risk areas depending on clinical suspicion
Isolation for confirmed positive patients OR highly symptomatic suspected / probable cases
These patients should be moved immediately to the isolation unit.
General practices and procedures
- Providers should move from asymptomatic to symptomatic and finally to confirmed patients
- Limit transport and movement of patients. When transport is necessary don clean PPE, place face mask on patient, and follow respiratory/hygiene etiquette
- The isolation area must be a separate enclosed space removed from other patients
- Equipment (stethoscope, BP cuff, pulse oximeter) must remain in the room and must be cleaned and disinfected between each patient (e.g., by using ethyl alcohol 70%)
- No visitors for suspected or confirmed patients (see exceptions below) as a strategy to help conserve PPE. All parents must wear PPE and can remain with a child as a caregiver
- Once patient is in the isolation area they cannot leave except to a dedicated bathroom for isolated patients, movement within the hospital per healthcare provider, or discharge
- Maintain a record of all persons entering a patient’s room or isolation space, including all staff and visitors
Covid-19 triage & screening flowcharts