Introduction / overview
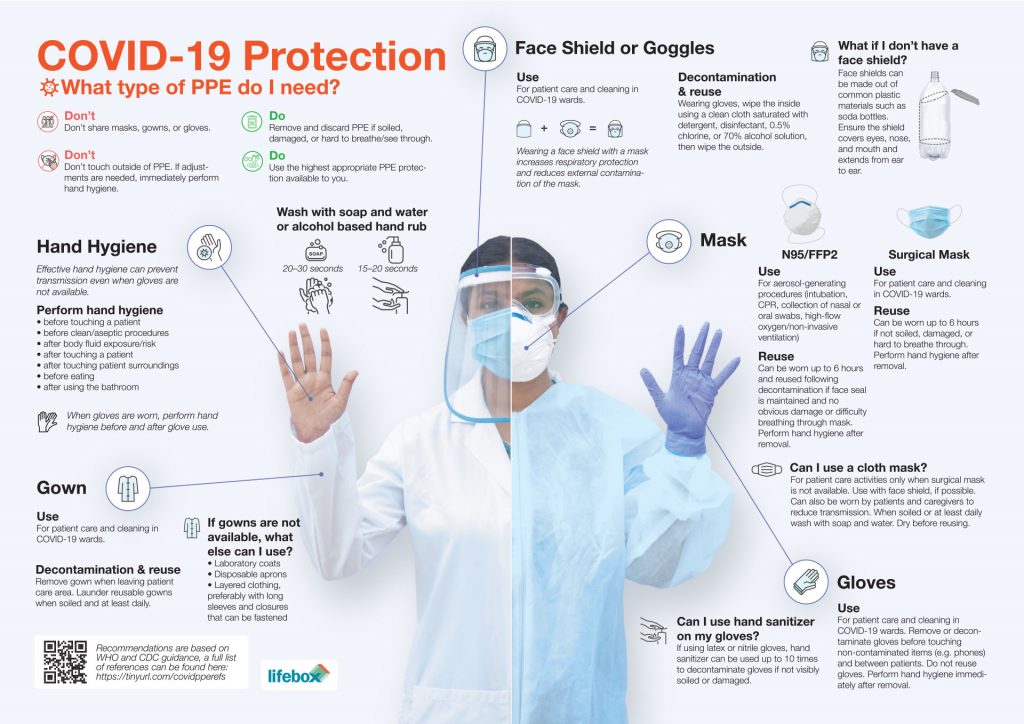
Access to adequate quantities and types of personal protective equipment (PPE) is an essential component of providing safe clinical care during the COVID-19 pandemic – essential for protecting yourself, your staff and your patients. This page lists the necessary equipment for implementing contact/droplet precautions in your healthcare facility.
Equipment needed
Eye and face protection
Eye and face protection provides protection against contamination to the eyes from respiratory droplets, aerosols arising from AGMPs and from splashing of secretions (including respiratory secretions), blood, or other bodily fluids.
Eye and face protection can be achieved by the use of any one of the following:
- Surgical mask with integrated visor
- Full face shield or visor
- Polycarbonate safety spectacles or equivalent
Regular corrective spectacles are not considered adequate eye protection.
While performing AGMPs, a full face shield or visor is recommended.

The same as for respirators and FRSMs, eye protection should: be well fitted; not be allowed to dangle after or between each use; not be touched once put on; be removed outside the patient room, cohort area or 2 metres away from possible or confirmed COVID-19 cases.
Disposable, single-use, eye and face protection is recommended for single or single session use and then is to be discarded as healthcare (clinical) waste. However, re-usable eye and face protection is acceptable if decontaminated between single or single session use, according to the manufacturer’s instructions or local infection control policy.
Goggles
It is important that the eye protection maintains its fit and function and remains tolerable for the user. Eye and face protection should be discarded and replaced and not be subject to continued use if damaged, soiled (for example, with bodily fluids) or uncomfortable.
Respirators
Respirators are used to prevent inhalation of small airborne particles arising from AGMPs. All respirators should:
- Be well fitted, covering both nose and mouth
- Not be allowed to dangle around the neck of the wearer after or between each use
- Not be touched once put on
- Be removed outside the patient room, cohort area or COVID-19 ward
Respirators can be single use or single session use (disposable) and fluid-resistant. Note that valved respirators are not fully fluid-resistant unless they are also ‘shrouded’. Valved, non-shrouded FFP3 respirators are not considered to be fluid resistant and therefore should be worn with a full face shield if splashing of blood or bodily fluids is anticipated.
FFP3 respirators filter at least 99% of airborne particles. The HSE states that all staff who are required to wear an FFP3 respirator must be fit tested for the relevant model to ensure an adequate seal or fit (according to the manufacturers’ guidance). Fit checking (according to the manufacturers’ guidance) is necessary when a respirator is donned to ensure an adequate seal has been achieved.
Masks


It is important to ensure that facial hair does not cross the respirator sealing surface and if the respirator has an exhalation valve, hair within the sealed mask area should not impinge upon or contact the valve. Respirators should be compatible with other facial protection used (protective eyewear) so that this does not interfere with the seal of the respiratory protection.
Coveralls


Disposable gloves
Disposable gloves must be worn when providing direct patient care and when exposure to blood and or other bodily fluids is anticipated or likely, including during equipment and environmental decontamination. Disposable gloves are subject to single use and must be disposed of immediately after completion of a procedure or task and after each patient contact, as per Standard Infection Control Precautions (SICPs), followed by hand hygiene. Double gloving is not necessary.



Disposable coveralls, aprons and gowns
Disposable plastic aprons must be worn to protect staff uniform or clothes from contamination when providing direct patient care and during environmental and equipment decontamination.
Disposable fluid repellent coveralls or long-sleeved gowns must be worn when a disposable plastic apron provides inadequate cover of staff uniform or clothes for the procedure or task being performed, and when there is a risk of splashing of bodily fluids such as during AGMPs in higher risk areas or in operative procedures. If non-fluid-resistant gowns are used, a disposable plastic apron should be worn. If extensive splashing is anticipated then use of additional fluid repellent items may be appropriate.
Disposable aprons are subject to single use and must be disposed of immediately after completion of a procedure or task and after each patient contact as per SICPs. Hand hygiene should be practiced as per SICPs and extended to exposed forearms. Disposable fluid repellent coveralls or long-sleeved gowns are for single use or for single session use in certain circumstances but should be discarded at the end of a session or earlier if damaged or soiled.

Boots

Sessional or single use PPE
Aprons and gloves are subject to single use as per SICPs, with disposal and hand hygiene after each patient contact.
Respirators, fluid-resistant (Type IIR) surgical masks (FRSM), eye protection and disposable fluid repellent coveralls or long-sleeved disposable fluid repellent gowns can be subject to single session use in certain circumstances .
A single session refers to a period of time where a healthcare worker is undertaking duties in a specific clinical care setting or exposure environment. For example, a session might comprise a ward round, or taking observations of several patients in a cohort bay or ward. A session ends when the healthcare worker leaves the clinical care setting or exposure environment. Once the PPE has been removed it should be disposed of safely. The duration of a single session will vary depending on the clinical activity being undertaken.
While generally considered good practice, there is no evidence to show that discarding disposable respirators, face masks or eye protection in between each patient reduces the risk of infection transmission to the healthcare worker or the patient. Indeed, frequent handling of this equipment to discard and replace it could theoretically increase risk of exposure in high demand environments, for example, by leading to increased face touching during removal. The rationale for recommending sessional use in certain circumstances is therefore to reduce risk of inadvertent indirect transmission, as well as to facilitate delivery of efficient clinical care.
PPE should not be subject to continued use if damaged, soiled, compromised or uncomfortable, and a session should be ended in these circumstances. While the duration of a session is not specified here, the duration of use of PPE items should not exceed manufacturer instructions. Appropriateness of single versus sessional use is dependent on the nature of the task or activity being undertaken and the local context.