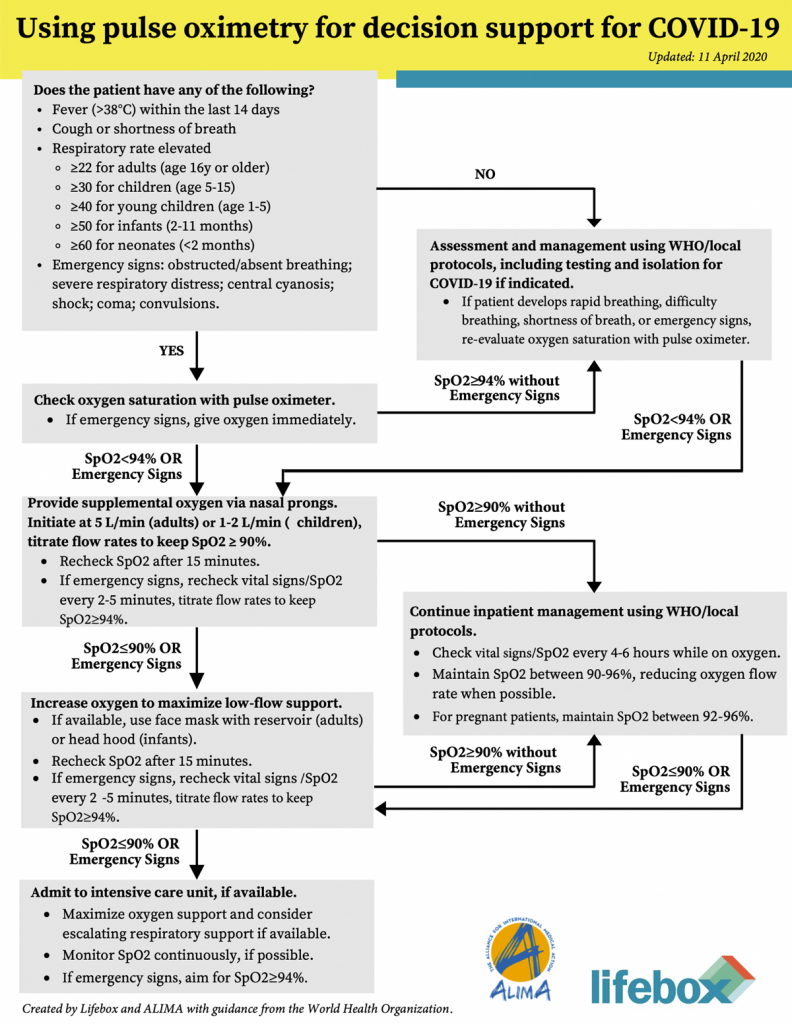
Pulse oximetry to detect early deterioration of patients with COVID-19 in primary and community care settings
A pulse oximeter measures oxygen saturation of haemoglobin in the blood by comparing the absorbance of light of different wavelengths across a translucent part of the body. Pulse oximetry is the best method available for detecting and monitoring an abnormally low concentration of oxygen in the blood (hypoxaemia).
Even the best combinations of clinical signs commonly lead to misdiagnosis of hypoxaemia in some patients with normal oxygen or fail to detect some hypoxaemic patients. Pulse oximetry should be performed on all patients with severe acute respiratory infection (SARI).
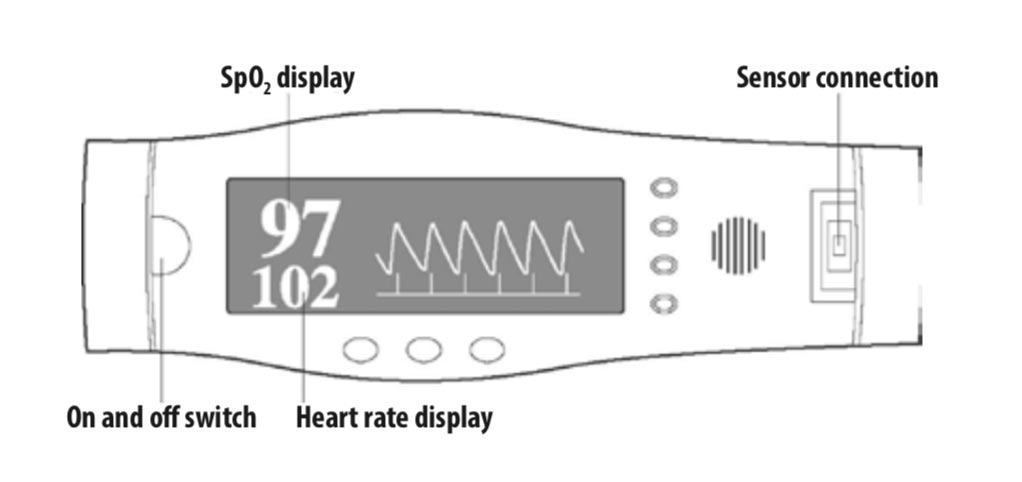
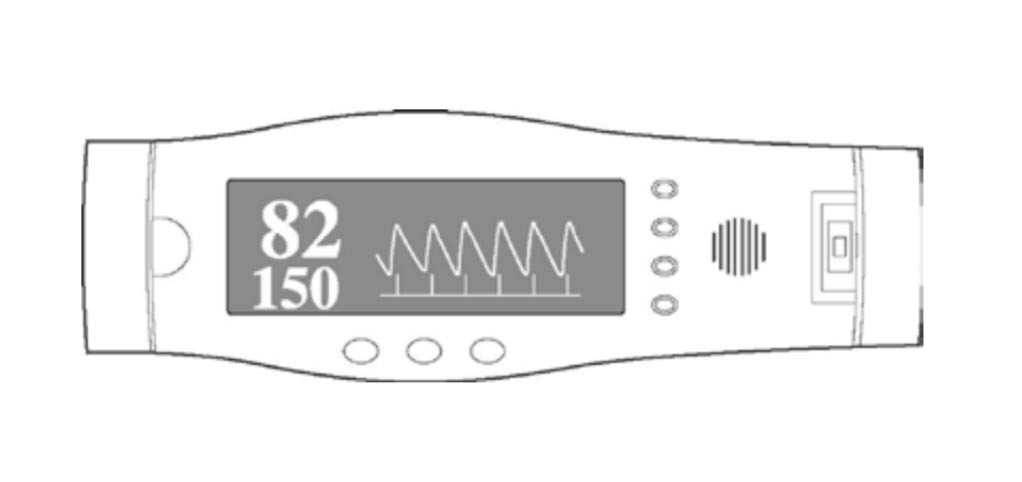
Examples of pulse oximeter displays showing normal and abnormal readings are given below.
Pulse oximeter displaying normal reading
This image shows a pulse oximeter with a normal reading (pulse rate = 102 BPM; SpO, = 97%) and a plethysmographic (pulse) wave indicating a good arterial trace and a valid reading.
Pulse oximeter displaying abnormal reading
In this image (pulse rate = 150 BPM; SpO, = 82%), the pulse oximeter has a good plethysmograpnic wave, indicating a valid arterial trace. Therefore, the SpO2, reading which is abnormally low (82%), is accurate and indicates that the patient is hypoxaemic. Oxygen should be given. Note the increased heart rate, which is common in seriously ill patients.
Video: Use of a pulse oximeter in the COVID-19 pandemic
What to do if you see a low oxygen reading?
Confirm hypoxia with pulse oximeter
- Start oxygen therapy if SpO2 < 90%. Use oxygen delivery device: nasal cannula (prongs) or nasal catheter or face mask
- Nasal prongs recommended for children < 5 years of age
- Keep simple surgical face mask on patient, over nasal prongs and under any type of oxygen face mask. This reduces viral spread to staff and other patients
- Adjust O2 flow to target SpO2 > 90% in adults & children. If signs of multi-organ failure including shock or alteration of mental status SpO2 > 94%. In pregnant patients target SpO2 > 92 – 95%
- If the target SpO2 > 90% cannot be achieved, or if SpO2 << 90%, suspect Acute Respiratory Distress Syndrome (ARDS). Consider nursing patient in the prone position for periods with a pillow under the chest. This may avoid the need for mechanical ventilation
- If the SpO2 does not improve, advanced oxygen therapy and mechanical ventilation are required. If possible these patients should to be moved to another ward for management with intubation, oxygenation and ventilation. IPAC measures with intubation, airway nursing care and ventilation are vital
Source: WFSA World Federation of ANESTHESIOLOGISTS | Link